

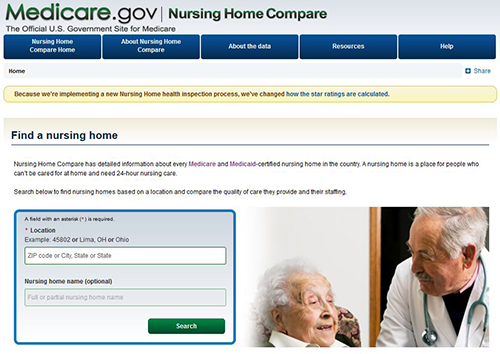
nursing homes on the quality of care they deliver on their website, Nursing Home Compare, in 2002. In an effort to improve quality in nursing homes, the CMS began publicly rating all U.S. If either of these effects is realized, quality will improve. Second, public reporting may increase the likelihood that patients select high-quality providers, thus increasing the number of patients receiving high-quality care. First, public reporting may motivate improvements in the quality of individual providers, increasing provider-specific quality of care. Public reporting is a frequently adopted policy initiative designed to improve health care quality in two ways ( 12). Rather, we focus on the set of process measures that are commonly used in nursing homes as the focus of state surveys of nursing home quality. Our goal is not to test an all-encompassing or exhaustive list of organizational changes that could lead to improved patient outcomes. We also take advantage of a public reporting initiative in nursing homes initiated by the Center for Medicare and Medicaid Services (CMS), Nursing Home Compare, as an exogenous source of outcome improvements in nursing homes to address potential endogeneity. Our objective in this paper is to test the extent to which improvements in outcomes of care are explained by changes in nursing home processes, a setting where, to our knowledge, this link has not been previously studied on a large scale.

Potential endogeneity also limits the conclusions as providers who perform well on process measures may also perform well on outcome measures for reasons other than a direct link between process and outcomes-other, unobserved factors may determine both types of performance. Prior work, primarily in the setting of hospitals ( 7, 8) and outpatient care ( 4, 5) has found small effects when using cross-sectional data to test the correlation between process and outcome measures.
However, establishing a link between process and outcomes measures has proven challenging. Linking processes and outcomes is thus a vital part of the quality-improvement agenda. For outcome measures to be effective tools for quality improvement, providers must know what processes affect patient outcomes and how these inputs can be targeted to improve outcomes. Unlike process measures, which can directly inform quality improvement activities, outcomes may be difficult to change and may be perceived as being somewhat beyond the control of the provider. However, disadvantages of tying incentives to outcome measures are often cited. This approach is being increasingly adopted across multiple health care settings, including hospitals, nursing homes, and home health agencies ( 9– 11). As a result, questions remain about whether measuring and providing incentives to improve processes of care will lead to improved patient outcomes.Īn alternative approach is to focus measurement and incentives directly on outcomes because this is the endpoint that patients care most about. Despite this evidence base, research on the effectiveness of these processes in real-world settings has found that improved processes do not always translate to improved outcomes at the individual ( 4– 6) or provider level ( 7, 8). Indeed, the use of processes of care is most often well supported by scientifically rigorous efficacy studies suggesting that if care is appropriately delivered, patient outcomes will improve ( 2, 3). Many quality measures focus on process of care with the implicit assumption, first noted by Donabedian, that improvements in process will lead to improvements in patient outcomes ( 1). Establishing a link between processes and outcomes of care has become an essential part of current efforts to improve health care quality.


 0 kommentar(er)
0 kommentar(er)
